Hemodialysis |
|
|
|
Purpose
Hemodialysis cleans and filters your blood using a machine to temporarily rid your body of harmful wastes, extra salt, and extra water. Hemodialysis helps control blood pressure and helps your body keep the proper balance of important chemicals such as potassium, sodium, calcium, and bicarbonate.
How It Works
Hemodialysis uses a special filter called a dialyzer that functions as an artificial kidney to clean your blood. During treatment, your blood travels through tubes into the dialyzer, which filters out wastes and extra water. Then the cleaned blood flows through another set of tubes back into your body. The dialyzer is connected to a machine that monitors blood flow and removes wastes from the blood.
Hemodialysis is usually needed three times a week.
Each treatment lasts from 3 to 5 or more hours. During treatment, you can read, write, sleep, talk, or watch TV.
Getting Ready
If you choose hemodialysis, several months before your first treatment, an access to your bloodstream will need to be created. You may need to stay overnight in the hospital, but many patients have their access placed on an outpatient basis. This access provides an efficient way for blood to be carried from your body to the dialysis machine and back without causing discomfort. The two main types
of access are a fistula and a graft.
Possible Complications
Vascular access problems are the most common reason for hospitalization among people on hemodialysis. Common problems include infection, blockage from clotting, and poor blood flow. These problems can keep your treatments from working. You may need to undergo repeated surgeries in order to get a properly functioning access.
Other problems can be caused by rapid changes in your body's water and chemical balance during treatment. Muscle cramps and hypotension, or a sudden drop in blood pressure, are two common side effects. Low blood pressure or hypotension can make you feel weak, dizzy, or sick to your stomach. You'll probably need a few months to adjust to hemodialysis. Side effects can often be treated quickly and easily, so you should always report them to your doctor and dialysis staff. You can avoid many side effects if you follow a proper diet, limit your liquid intake, and take your medicines as directed.
|
|
Adjusting to Changes
Even in the best situations, adjusting to the effects of kidney failure and the time you spend on dialysis can be difficult. Aside from the "lost time," you may have less energy. You may need to make changes in your work or home life, giving up some activities and responsibilities. Keeping the same schedule you kept when your kidneys were working can be very difficult now that your kidneys have failed. Accepting this new reality can be very hard on you and your family. A counselor or social worker can help you cope.
Many patients feel depressed when starting dialysis, or after several months of treatment. If you feel depressed, you should talk with your social worker, nurse, or doctor because this is a common problem that can often be treated effectively.
Who Performs It
Hemodialysis is usually done in a dialysis center by nurses and trained technicians. In some parts of the country, it can be done at home with the help of a partner, usually a family member or friend. If you decide to do home dialysis, you and your partner will receive special training.
Diet for Hemodialysis
Hemodialysis and a proper diet help reduce the wastes that build up in your blood. A dietitian is available at all dialysis centers to help you plan meals according to your doctor's orders. When choosing foods, you should remember to
- Eat balanced amounts of high-protein foods such as meat, chicken, and fish.
- Control the amount of potassium you eat. Potassium is a mineral found in salt substitutes, some fruits (bananas, oranges), vegetables, chocolate, and nuts. Too much potassium can be dangerous.
- Limit how much you drink. When your kidneys aren't working, water builds up quickly in your body. Too much liquid makes your tissues swell and can lead to high blood pressure, heart trouble, and cramps and low blood pressure during dialysis.
- Avoid salt. Salty foods make you thirsty and make your body hold water.
- Limit foods such as milk, cheese, nuts, dried beans, and dark colas. These foods contain large amounts of the mineral phosphorus. Too much phosphorus in your blood causes calcium to be pulled from your bones, which makes them weak and brittle and can cause arthritis. To prevent bone problems, your doctor may give you special medicines, which you must take with meals every day as directed.
|
| |
| |
|
| |
Pros |
|
Cons |
| In the centre : |
-
Facilities are widely available.
-
You have trained professionals with you at all times.
-
You can get to know other patients.
|
|
-
Treatments are scheduled by the center and are relatively fixed
-
You must travel to the center for treatment
|
| At home : |
-
You can do it at the times you choose (but you still must do it as often as your doctor orders)
-
You don't have to travel to a center
-
You gain a sense of independence and control over your treatment
|
|
-
You must have a helper
-
Helping with treatments may be stressful to your family
-
You and your helper need training
-
You need space for storing the machine and supplies at home
|
| |
|
| |
Questions to ask:
- Is hemodialysis the best treatment choice for me? Why?
- If I'm treated at a center, can I go to the center of my choice?
- What should I look for in a dialysis center?
- Will my kidney doctor see me at dialysis?
- What does hemodialysis feel like?
- What is self-care dialysis?
- Is home hemodialysis available in my area? How long does it take to learn? Who will train my partner and me?
|
|
- What kind of blood access is best for me?
- As a hemodialysis patient, will I be able to keep working? Can I have treatments at night?
- How much should I exercise?
- Who will be on my health care team? How can these people help me?
- Whom can I talk with about finances, sexuality, or family concerns?
- How/where can I talk to other people who have faced this decision?
|
| |
Back to menu |
|
|
Peritoneal Dialysis |
|
|
Purpose
Peritoneal dialysis is another procedure that removes extra water, wastes, and chemicals from your body. This type of dialysis uses the lining of your abdomen to filter your blood. This lining is called the peritoneal membrane and acts as the artificial kidney.
How It Works
A mixture of minerals and sugar dissolved in water, called dialysis solution, travels through a soft tube into your abdomen. The sugar, called dextrose, draws wastes, chemicals, and extra water from the tiny blood vessels in your peritoneal membrane into the dialysis solution. After several hours, the used solution is drained from your abdomen through the tube, taking the wastes from your blood with it. Then you fill your abdomen with fresh dialysis solution, and the cycle is repeated. Each cycle is called an exchange.
Getting Ready
Before your first treatment, a surgeon places a small, soft tube called a catheter into your abdomen. The catheter tends to work better if there is adequate time--usually from 10 days to 2 or 3 weeks--for the insertion site to heal. This is another way in which planning your dialysis access can improve treatment success. This catheter stays there permanently to help transport the dialysis solution to and from your abdomen.
Who Performs It
Both types of peritoneal dialysis are usually performed by the patient without help from a partner. CAPD is a form of self-treatment that needs no machine. However, with CCPD, you need a machine to drain and refill your abdomen.
Possible Complications
The most common problem with peritoneal dialysis is peritonitis, a serious abdominal infection. This infection can occur if the opening where the catheter enters your body becomes infected or if contamination occurs as the catheter is connected or disconnected from the bags. Peritonitis requires antibiotic treatment by your doctor.
To avoid peritonitis, you must be careful to follow procedures exactly and learn to recognize the early signs of peritonitis, which include fever, unusual color or cloudiness of the used fluid, and redness or pain around the catheter. Report these signs to your doctor immediately so that peritonitis can be treated quickly to avoid serious problems. |
|
Types of Peritoneal Dialysis
There are three types of peritoneal dialysis.
1. Continuous Ambulatory Peritoneal Dialysis (CAPD)
CAPD is the most common type of peritoneal dialysis. It requires no machine and can be done in any clean, well-lit place. With CAPD, your blood is always being cleaned. The dialysis solution passes from a plastic bag through the catheter and into your abdomen, where it stays for several hours with the catheter sealed. The period that dialysis solution is in your abdomen is called the dwell time. Next, you drain the dialysis solution back into the bag for disposal. You then use the same catheter to refill your abdomen with fresh dialysis solution so the cleaning process can begin again. With CAPD, the dialysis solution stays in your abdomen for a dwell time of 4 to 6 hours (or more). The process of draining the used dialysis solution and replacing it with fresh solution takes about 30 to 40 minutes. Most people change the dialysis solution at least four times a day and sleep with solution in their abdomen at night. With CAPD, it's not necessary to wake up and perform dialysis tasks during the night.
2. Continuous Cycler-Assisted Peritoneal Dialysis (CCPD)
CCPD uses a machine called a cycler to fill and empty your abdomen three to five times during the night while you sleep. In the morning, you begin one exchange with a dwell time that lasts the entire day. You may do an additional exchange in the middle of the afternoon without the cycler to increase the amount of waste removed and to reduce the amount of fluid left behind in your body.
3. Combination of CAPD and CCPD
If you weigh more than 175 pounds or if your peritoneum filters wastes slowly, you may need a combination of CAPD and CCPD to get the right dialysis dose. For example, some people use a cycler at night but also perform one exchange during the day. Others do four exchanges during the day and use a minicycler to perform one or more exchanges during the night. You'll work with your health care team to determine the best schedule for you.
Diet for Peritoneal Dialysis
A peritoneal dialysis diet is slightly different from a hemodialysis diet.
- You'll still need to limit salt and liquids, but you may be able to have more of each, compared with hemodialysis.
- You must eat more protein.
- You may have different restrictions on potassium.
- You may need to cut back on the number of calories you eat because there are calories in the dialysis fluid that may cause you to gain weight.
Your doctor and a dietitian who specializes in helping people with kidney failure will be able to help you plan your meals.
|
| |
|
| |
Pros |
|
Cons |
| CAPD : |
- You can do it alone.
- You can do it at times you choose as long as you perform the required number of exchanges
each day.
- You can do it in many locations.
- You don't need a machine.
|
|
- It can disrupt your daily schedule.
- This is a continuous treatment & all exchanges must be performed 7 days a week.
. |
| CCPD : |
- You can do it at night, mainly while you are sleeping.
|
|
|
| |
|
| |
Questions to ask:
- Is peritoneal dialysis the best treatment choice for me? Why? If yes, which type is best?
- How long will it take me to learn how to do peritoneal dialysis?
- What does peritoneal dialysis feel like?
- How will peritoneal dialysis affect my blood pressure?
- How will I know if I have peritonitis? How is it treated?
- As a peritoneal dialysis patient, will I be able to continue working?
|
|
- How much should I exercise?
- Where do I store supplies?
- How often do I see my doctor?
- Who will be on my health care team? How can these people help me?
- Whom do I contact with problems?
- Whom can I talk with about finances, sexuality, or family concerns?
- How/where can I talk to other people who have faced this decision?
|
| |
Back to menu |
|
|
Transplantation |
|
|
If you have advanced and permanent kidney failure, kidney transplantation may be the treatment option that allows you to live much like you lived before your kidneys failed. Since the 1950s, when the first kidney transplants were performed, we've learned much about how to prevent rejection and minimize the side effects of medicines.
But transplantation is not a cure; it's an ongoing treatment that requires you to take medicines for the rest of your life and the wait for a donated kidney can be years long.
A successful transplant takes a coordinated effort from your whole health care team, including your nephrologist, transplant surgeon, transplant coordinator, pharmacist, dietitian, and social worker. The most important members of your health care team are you and your family. By learning about your treatment, you can work with your health care team to give yourself the best possible results, and you can lead a full, active life.
Getting Ready
The transplantation process has many steps. First, talk with your doctor, because transplantation isn't for everyone. Your doctor may tell you that you have a condition that would make transplantation dangerous or unlikely to succeed.
You may receive a kidney from a member of your family (living, related donor), from a person who has recently died (cadaveric donor), or sometimes from a spouse or a very close friend (living, unrelated donor). If you don't have a living donor, you're placed on a waiting list for a cadaveric kidney. The wait for a cadaveric donor kidney can be several years.
The transplant team considers three factors in matching kidneys with potential recipients. These factors help predict whether your body's immune system will accept the new kidney or reject it. |
|
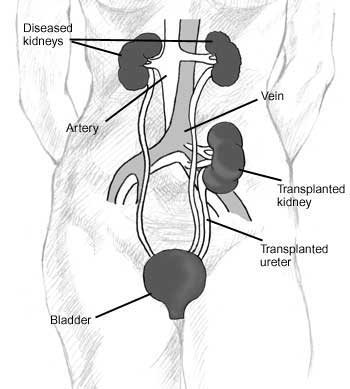
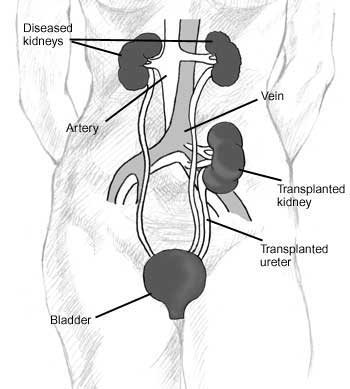
How It Works
Kidney transplantation is a procedure that places a healthy kidney from another person into your body. This one new kidney takes over the work of your two failed kidneys.
A surgeon places the new kidney inside your lower abdomen and connects the artery and vein of the new kidney to your artery and vein. Your blood flows through the new kidney, which makes urine, just like your own kidneys did when they were healthy. Unless they are causing infection or high blood pressure, your own kidneys are left in place.
 |
| |
- Blood type. Your blood type (A, B, AB, or O) must match the donor's. This is the most important matching factor.
- Human leukocyte antigens (HLAs). Your cells carry six important HLAs, three inherited from each parent. Family members are most likely to have a complete match. You may still receive a kidney if the HLAs aren't a complete match as long as your blood type matches the organ donor's and other tests are negative.
- Cross-matching antigens. The last test before implanting an organ is the cross-match. A small sample of your blood will be mixed with a sample of the organ donor's blood in a tube to see if there's a reaction. If no reaction occurs, the result is called a negative cross-match, and the transplant operation can proceed.
Possible Complications
Transplantation is the closest thing to a cure. But no matter how good the match, your body may reject your new kidney. A common cause of rejection is not taking medication as prescribed.
Your doctor will give you drugs called immunosuppressants to help prevent your body's immune system from attacking the kidney, a process called rejection. You'll need to take immunosuppressants every day for as long as the transplanted kidney is functioning. Sometimes, however, even these drugs can't stop your body from rejecting the new kidney. If this happens, you'll go back to some form of dialysis and possibly wait for another transplant. |
|
The Time It Takes
How long you'll have to wait for a kidney varies. Because there aren't enough cadaveric donors for every person who needs a transplant, you must be placed on a waiting list. However, if a voluntary donor gives you a kidney, the transplant can be scheduled as soon as you're both ready. Avoiding the long wait is a major advantage of living donation.
The surgery takes 3 to 4 hours. The usual hospital stay is about a week. After you leave the hospital, you'll have regular followup visits.
If someone has given you a kidney, the donor will probably stay in the hospital about the same amount of time. However, a new technique for removing a kidney for donation uses a smaller incision and may make it possible for the donor to leave the hospital in 2 to 3 days.
Between 85 and 90 percent of transplants from cadaveric donors are working 1 year after surgery. Transplants from living relatives often work better than transplants from cadaveric donors because they're usually a closer match.
Diet for Transplantation
Diet for transplant patients is less limited than it is for dialysis patients, although you may still have to cut back on some foods. Your diet will probably change as your medicines, blood values, weight, and blood pressure change.
- You may need to count calories. Your medicine may give you a bigger appetite and cause you to gain weight.
- You may have to eat less salt. Your medications may cause your body to retain sodium, leading to high blood pressure.
|
Immunosuppressants can weaken your immune system, which can lead to infections. Some drugs may also change your appearance. Your face may get fuller; you may gain weight or develop acne or facial hair. Not all patients have these problems, though, and diet and makeup can help.
Immunosuppressants work by diminishing the ability of immune cells to function. In some patients, over long periods of time, this diminished immunity can increase the risk of developing cancer. Some immunosuppressants can cause cataracts, diabetes, extra stomach acid, high blood pressure, and bone disease. When used over time, these drugs may also cause liver or kidney damage in a few patients. |
| |
|
| |
Pros |
|
Cons |
| Kidney Transplant : |
|
|
|
| |
|
| |
Back to menu |
|
|
Refusing or withdarwing from treatment
|
| |
For many people, dialysis and transplantation not only extend life but also improve quality of life. For others who have serious ailments in addition to kidney failure, dialysis may seem a burden that only prolongs suffering. You have the right to refuse or withdraw from dialysis if you feel you have no hope of leading a life with dignity and meaning. You may want to speak with your spouse, family, religious counselor, or social worker as you make this decision.
If you withdraw from dialysis treatments or refuse to begin them, you may live for a few days or for several weeks, depending on your health and your remaining kidney function. Your doctor can give you medicines to make you more comfortable during this period. Should you change your mind about refusing dialysis, you may start or resume your treatments at any time.
|
|
An advance directive may be a living will, a document that details the conditions under which you would want to refuse treatment. You may state that you want your health care team to use all available means to sustain your life. Or you may direct that you be withdrawn from dialysis if you become permanently unresponsive or fall into a coma from which you won't awake. In addition to dialysis, other life-sustaining treatments that you may choose or refuse include
- Cardiopulmonary resuscitation (CPR)
- Tube feedings
- Mechanical or artificial respiration
- Antibiotics
- Surgery
- Blood transfusions
Another form of advance directive is called a durable power of attorney for health care decisions or a health care proxy. In this type of advance directive, you assign a person to make health care decisions for you if you become unable to make them for yourself. Make sure the person you name understands your values and is willing to follow through on your instructions. |
| |
Even if you're satisfied with your quality of life on dialysis, you should think about circumstances that might make you want to stop dialysis treatments. At some point in a medical crisis, you might lose the ability to express your wishes to your doctor. An advance directive is a statement or document in which you give instructions either to withhold treatment or to provide it, depending on your wishes and the specific circumstances. |
| |
|
|
|
| |
Back to menu |
|
|
| |
|
Conclusion
|
|
|
| |
Deciding which type of treatment is best for you isn't easy. Your decision depends on your medical condition, lifestyle, and personal likes and dislikes. Discuss the pros and cons of each treatment with your health care team and family. You can switch between treatment methods during the course of your therapy. If you start one form of treatment and decide you'd like to try another, talk to your doctor. The key is to learn as much as you can about your choices first. With that knowledge, you and your doctor will choose the treatment that suits you best.
|
| |
Additional Reading |
|
|
| |
AAKP Patient Plan,
Renalife (published quarterly)
This is a series of booklets and newsletters that cover the different phases of learning about kidney failure, choosing a treatment, and adjusting to changes.
American Association of Kidney Patients
100 South Ashley Drive
Suite 280
Tampa, FL 33602
Phone: 1-800-749-2257 or (813) 223-7099
AAKPnat@aol.com
www.aakp.org
|
|
Financing Transplantation: What Every
Patient Needs To Know,
2nd edition, 1996
United Network for Organ Sharing
1100 Boulders Parkway
Suite 500
P.O. Box 13770
Richmond, VA 23225-8770
Phone: 1-888-894-6361 to order single copies
(804) 330-8541 to order bulk copies
www.unos.org |
| |
Kidney Disease: A Guide for Patients and Their Families
American Kidney Fund
6110 Executive Boulevard
Suite 1010
Rockville, MD 20852
Phone: 1-800-638-8299 or (301) 881-3052
helpline@akfinc.org
www.akfinc.org
|
|
National Kidney Foundation (NKF) Patient Education Brochures
Family Focus Newsletter
(includes materials based on NKF's Dialysis Outcomes Quality Initiative)
National Kidney Foundation, Inc.
30 East 33rd Street
New York, NY 10016
Phone: 1-800-622-9010 or (212) 889-2210
www.kidney.org |
| |
Many thanks to the NIDDK for making this information available.
|
| |
The National Institute of Diabetes and Digestive and Kidney Diseases thanks these dedicated health professionals for their careful review of this publication:
William Owen Jr., M.D.
Duke University Medical Center
Richard D. Swartz, M.D.
University of Michigan Health System |
|
The individuals listed here facilitated field testing for this publication. NIDDK thanks them for their contribution:
Kim Bayer, M.A., R.D., L.D.
BMA Dialysis
Bethesda, MD
Cora Benedicto, R.N.
Clinic Director
Gambro Health Care
N Street Clinic
Washington, DC |
| |
|
| |
Back to menu |
|
|
|
 |
| incorporated association not for gain registration no: 1977/002650/08 |
Website powered by  |
Kwa Zulu Natal Kidney Association,
P.O.Box 1332, Durban, 4000, ajfa@iafrica.com |
|